IN THIS LESSON
Topics Covered:
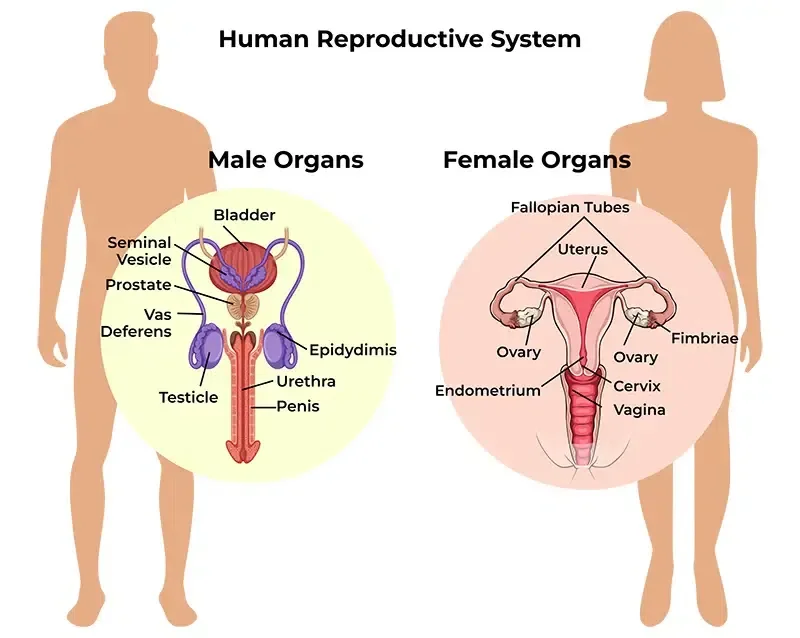
1. Female & Male Reproductive Anatomy
Learn the essential structures involved in conception, including ovaries, fallopian tubes, uterus, testes, and sperm pathways. This helps you understand how each part contributes to fertility.
2. Hormonal Regulation & Cycle Coordination
Explore how hormones like estrogen, progesterone, LH, and FSH regulate ovulation, menstruation, and sperm production. Understanding this cycle is key to explaining fertile windows.
3. How Reproduction Supports Conception
Discover how ovulation, egg quality, sperm development, and cervical fluid work together. This foundation highlights the biological steps required for successful fertilization.
Introduction
Understanding how the reproductive system works is one of the most empowering steps you can take on your fertility journey. In this lesson, we’ll break down the essential anatomy of both female and male reproductive systems, explaining what each organ does and how these structures work together during conception. You’ll also learn how hormones like estrogen, progesterone, LH, and FSH coordinate cycles, trigger ovulation, and support sperm production—insight that helps make sense of fertile windows and timing. Finally, we’ll explore how ovulation, egg quality, sperm health, and even cervical fluid play a role in helping pregnancy occur. By the end of this lesson, you’ll have a clear, science-based understanding of what needs to happen behind the scenes for conception to take place—knowledge that lays the foundation for everything else you’ll learn in this course.
1. Female & Male Reproductive Anatomy
A. FOUNDATIONAL DEFINITION & EXPLANATION
The reproductive system is composed of organs, structures, and pathways that work together to enable conception, pregnancy, and birth. Although often described separately as “female” or “male,” both systems function as interconnected counterparts designed to support fertilization. In individuals with ovaries, the reproductive system includes the ovaries, fallopian tubes, uterus, cervix, and vagina. In individuals with testes, the system includes the testes, epididymis, vas deferens, penis, and the glands that contribute to semen production. Understanding how these organs interact lays the foundation for supporting clients through fertility awareness, conception, and reproductive health decision-making.
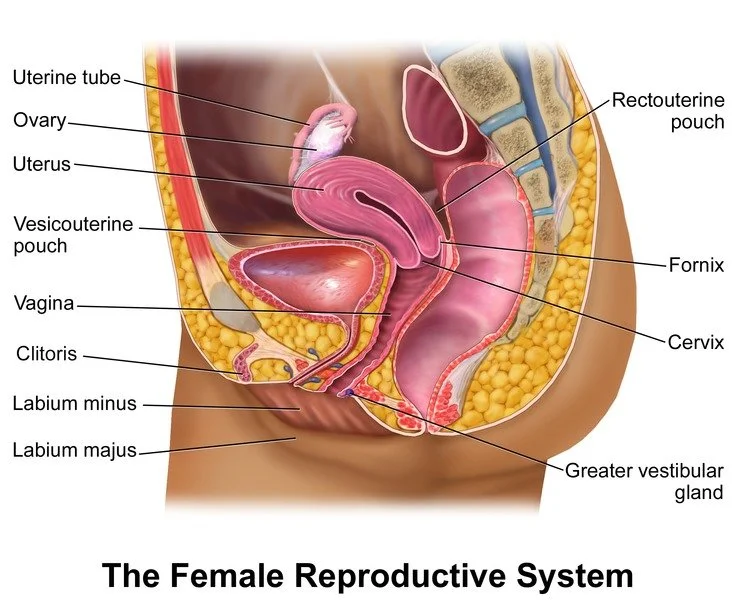
In ovary-bearing individuals, ovaries contain thousands of follicles—each with the potential to release an egg during the menstrual cycle. Once an egg matures, it is released into the fallopian tube in a process known as ovulation. Fertilization typically occurs inside the fallopian tube, where sperm and egg meet. From there, the fertilized egg (zygote) travels to the uterus and implants in the uterine lining. A real-world example is to imagine the reproductive system as a relay race: the ovary hands off the egg to the tube, the tube carries it safely along, and the uterus prepares a “landing zone.” If any portion of this relay is disrupted, conception becomes more challenging.
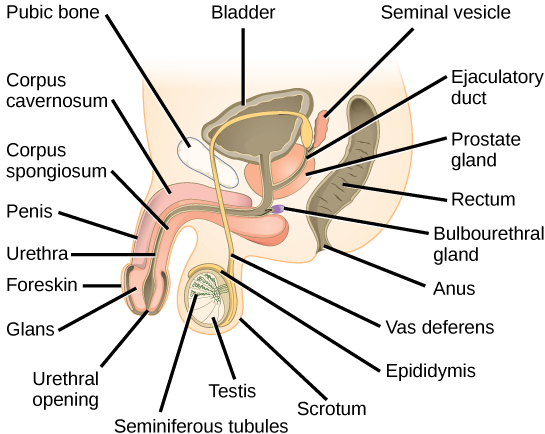
For individuals with testes, the primary reproductive organs are the testes, which produce both sperm and testosterone. Sperm develop in coiled structures called seminiferous tubules before moving to the epididymis for maturation. During ejaculation, sperm travel through the vas deferens, mix with seminal fluid from the prostate and seminal vesicles, and exit through the urethra. A helpful analogy is to think of the testes as “factories,” the epididymis as “quality control,” and the vas deferens as the “delivery route.” Each step contributes to the overall capacity for successful conception.
Both reproductive systems rely heavily on structural integrity for normal function. For example, blocked fallopian tubes can prevent egg–sperm interaction, while varicocele (enlarged veins around the testes) can affect sperm quality. Similarly, uterine abnormalities—such as fibroids or a septate uterus—may impact implantation or pregnancy continuation. These structural concerns highlight how anatomy and fertility are intertwined, reminding coaches that many reproductive issues involve multiple factors rather than a single “cause.”
Understanding reproductive anatomy also improves a fertility coach’s ability to explain common concerns in simple, empowering language. Instead of viewing anatomy as rigid or technical, students can help clients understand their bodies as dynamic systems capable of change, healing, and adaptation. Whether explaining how the cervix changes during the cycle, how sperm navigate the reproductive tract, or why pelvic infections sometimes affect fertility, a coach’s knowledge fosters clarity and confidence. Ultimately, a strong grounding in anatomy supports informed decision-making, reduces fear, and enhances communication between clients and their healthcare providers.
B. SCENARIOS & TIPS
Scenario 1: Client Confused About Why Anatomy Affects Conception
Your client is trying to conceive and feels frustrated that it hasn’t happened yet. They say they “feel healthy” and don’t understand why reproductive anatomy matters. They express confusion over how eggs and sperm actually meet inside the body. They look to you for clarity and reassurance.
Coach Response
“It makes complete sense that this feels confusing—so much of what happens inside the reproductive system occurs quietly and invisibly. Your body has a series of organs that all work together, and each one plays a specific role in helping sperm and egg meet. The ovaries release an egg, the fallopian tubes act like pathways, and the uterus prepares a space that can nurture a pregnancy. When we break it down step by step, it becomes a lot easier to understand.”
“One thing I like to remind clients is that even when everything is functioning normally, conception often takes time. The egg is only available for a short window, and sperm must swim through several anatomical structures to reach it. Nothing you’re experiencing suggests that your body isn’t capable—it simply means we are learning more about your unique rhythm. I can walk you through each part of the system so you feel more grounded and confident moving forward.”
Tips
This script is effective because it normalizes confusion while offering clear, non-clinical explanations. Clients often don’t receive this foundational education from healthcare providers, so simplicity and reassurance reduce anxiety. Coaches should avoid diagnosing or speculating about fertility conditions. Instead, reinforce body awareness and emphasize that anatomy varies from person to person. Encourage clients to observe their cycles and communicate openly with providers if they have questions. The goal is to empower rather than alarm.
Scenario 2: Partner Worried Their Anatomy Is the “Problem”
A partner expresses concern that their anatomy may be preventing conception. They mention long hours of sitting, tight clothing, or past injuries. They feel embarrassed to bring it up and fear being judged. They ask whether this could “all be my fault.”
Coach Response
“Thank you for sharing that—it takes a lot of courage to talk openly about reproductive health. Many people are surprised to learn how sensitive sperm production is to everyday things like heat, long sitting, or even stress. These factors don’t mean anything is wrong with your anatomy; rather, they reflect how responsive the reproductive system is to the environment.”
“Anatomy is only one piece of the bigger fertility picture, and it’s rare for conception challenges to fall entirely on one partner. Lifestyle adjustments can often support sperm health, and many changes are reversible. You’re not alone in this, and there are simple steps you can explore without pressure. I’m here to support both of you equally as you navigate this journey.”
Tips
This response diffuses blame and reinforces partnership. Coaches must balance honesty with reassurance, reminding clients that sperm quality naturally fluctuates. Avoid interpreting semen analyses or suggesting medical diagnoses. Instead, focus on supportive language that encourages communication and shared responsibility. Offering practical, low-stress suggestions—like movement breaks or avoiding prolonged heat exposure—helps clients feel empowered rather than discouraged. Your role is to support understanding, not to assign fault.
Scenario 3: Client Concerned About Past Pelvic Infection or Surgery
A client shares that they previously had pelvic inflammatory disease (PID) or pelvic surgery and fears it may have damaged their reproductive organs. They worry that their fallopian tubes might be scarred or blocked. They feel overwhelmed and are scared to seek medical evaluation. They ask you if pregnancy is still possible.
Coach Response
“I’m really glad you brought this up—carrying fear alone can feel incredibly isolating. Many people with a history of infection or surgery go on to conceive without difficulty, especially when the issue was treated early. The reproductive system is remarkably resilient. At the same time, it’s completely valid to want reassurance and clarity.”
“A healthcare provider can offer specific testing to evaluate your fallopian tubes or uterus if that becomes necessary. My role is to support you emotionally as you gather information, not to assume something is wrong. You deserve to feel informed and empowered, and we can take this one step at a time. You’re not alone in this, and nothing about your history defines your future.”
Tips
Clients often assume worst-case scenarios when they hear terms like “PID” or “scar tissue.” A coach’s calm presence helps reduce panic and build trust. Avoid dismissing concerns or minimizing past experiences; instead, validate their feelings while encouraging evidence-based evaluation. Remind them that many reproductive issues have solutions or workarounds. Encourage small, manageable steps toward seeking care. Emphasize resilience and support throughout the process.
C. EVIDENCE-BASED INSIGHTS
Research 1: Fallopian Tube Motility and Fertility (Zhang et al., 2018)
Zhang and colleagues (2018) investigated how fallopian tubes actively move eggs and sperm rather than simply serving as passive channels. The researchers found that tiny hair-like cilia inside the tubes beat in coordinated patterns that propel the egg toward the uterus. They also discovered that muscular contractions within the tube assist sperm migration, especially during the fertile window. When infection or inflammation damages these cilia, egg transport becomes slower and less coordinated. The study highlighted that even mild inflammation can disrupt normal function. These findings help explain why past pelvic infections sometimes affect conception. The research also emphasizes the importance of early diagnosis and treatment for reproductive tract infections. For coaches, this study provides a clear way to explain how delicate and essential the tubes are. It confirms that anatomy and reproductive health are deeply interconnected.
Research 2: Testicular Heat Exposure and Sperm Quality (Hamada et al., 2020)
Hamada et al. (2020) examined how heat affects sperm development in individuals with testes. The researchers discovered that sperm production requires a temperature slightly lower than core body temperature, which is why the scrotum hangs outside the body. Frequent exposure to heat—such as hot tubs, saunas, heated car seats, or laptops placed on the lap—temporarily lowers sperm count and motility. These effects were shown to be reversible after several weeks of cooler exposure. The study also demonstrated significant improvement in sperm quality when heat exposure decreased. This suggests that simple lifestyle shifts can support reproductive health. The findings help reduce unnecessary fear by clarifying that many changes are temporary. For coaches, this research serves as a practical tool when advising clients about environmental impacts on fertility. It also reinforces the importance of supporting partners as part of the conception process.
Research 3: Uterine Structure and Implantation Outcomes (Liu et al., 2019)
Liu et al. (2019) explored how variations in uterine anatomy influence implantation and early pregnancy success. They found that a healthy endometrial lining, supported by adequate blood flow, is essential for an embryo to attach. Structural differences such as fibroids, polyps, or a septate uterus were associated with reduced implantation rates. However, the researchers emphasized that many anatomical variations are treatable or manageable. The study also found that hormonal balance influences how the uterine lining develops each cycle. Stress, sleep disturbances, and inflammation can indirectly affect the uterine environment. These findings highlight the interconnected nature of hormones, anatomy, and reproductive health. The study reassures clients that anatomical issues are not uncommon and that many individuals with these conditions conceive successfully. For coaches, this research offers a balanced, evidence-based explanation connecting anatomy with pregnancy outcomes.
D. KEY TERMS & DEFINITIONS
Fallopian Tubes
Fallopian tubes are two slender structures that connect the ovaries to the uterus. They are the site where fertilization typically occurs. Tiny hair-like cilia inside the tubes help move the egg toward the uterus. When inflammation or scarring damages these structures, it can affect egg transport. Blocked tubes are a common, treatable cause of infertility. Healthy tube function is essential for natural conception.
Ovaries
Ovaries store thousands of follicles, each capable of developing into a mature egg. They produce the hormones estrogen and progesterone, which regulate the menstrual cycle. Each month, one ovary typically releases an egg during ovulation. Ovarian health influences fertility, cycle regularity, and hormone balance. Conditions such as PCOS or diminished ovarian reserve can affect ovarian function. Understanding the ovaries helps clients grasp how eggs develop and mature.
Testes
The testes are the primary reproductive organs in individuals with testes, responsible for producing sperm and testosterone. Sperm develop in seminiferous tubules and mature in the epididymis. Testicular temperature plays a major role in sperm health. Injuries, infections, or heat exposure can temporarily affect sperm production. Testosterone from the testes influences libido, muscle mass, and overall reproductive function. Healthy testicular function supports both fertility and hormonal balance.
Uterus
The uterus is a muscular organ designed to support embryo implantation and fetal development. Its lining thickens each cycle in preparation for pregnancy. If no pregnancy occurs, the lining sheds during menstruation. Structural variations such as fibroids or polyps can influence pregnancy outcomes. The uterus expands dramatically during pregnancy to accommodate fetal growth. Understanding uterine anatomy helps coaches explain early pregnancy experiences.
Cervix
The cervix is the lower portion of the uterus that opens into the vagina. It produces cervical mucus, which changes texture throughout the menstrual cycle. Around ovulation, the cervix softens and mucus becomes more sperm-friendly. During labor, the cervix dilates to allow for birth. Past infections or surgical procedures can affect cervical function. Knowledge of cervical changes helps coaches support clients tracking fertility.
Vas Deferens
The vas deferens is a muscular tube that transports sperm from the epididymis to the urethra during ejaculation. It plays a key role in delivering sperm effectively. Blockages or surgical alterations—such as vasectomy—affect this transport. The vas deferens is part of a coordinated network that ensures sperm mix with seminal fluid. Understanding its function helps coaches explain male fertility pathways. It also clarifies how sperm reach the egg.
FAQs: Female & Male Reproductive Anatomy
-
A regular period is a good sign that the reproductive system is cycling predictably, but it doesn’t guarantee that every part of the anatomy is functioning perfectly. Regular bleeding does not always mean ovulation is happening, as some people experience “withdrawal bleeds” or anovulatory cycles. Even with normal cycles, factors like fallopian tube health, uterine lining quality, or sperm interactions can still affect fertility. The ovaries, uterus, cervix, and tubes all play unique roles, and issues in any of these structures may not be reflected in cycle regularity. Understanding the full reproductive system helps clients see the bigger picture beyond just periods.
Suggestions for Fertility Coach:
Reassure the client with a script such as, “A regular cycle is a great foundation, but it’s only one piece of the fertility picture.” Introduce the idea of tracking ovulation to understand the cycle more accurately. Suggest tools like LH strips, cervical mucus tracking, or basal temperature. Gently ask, “Have you noticed any signs that ovulation is happening each cycle?” Avoid alarming them; instead emphasize clarity: “Regular cycles are helpful, but anatomy and hormones work together—we just want to make sure all the steps are lining up.” Recommend a provider evaluation if irregularities or concerns arise. Normalize the learning process: “Most people don’t discover how their reproductive system works until they start trying to conceive.” Offer to help them map out the anatomy visually. End with supportive encouragement: “You’re already starting in a great place—we’re just adding information to make your path clearer.” -
The fallopian tubes are the pathway where sperm meet the egg and where fertilization usually occurs. If one tube is blocked, the egg from that side cannot travel toward the uterus, and sperm cannot reach it. However, if the other tube is open, conception is still possible because ovulation alternates sides in many (but not all) cycles. When both tubes are blocked, the egg and sperm cannot meet, making natural conception extremely unlikely. Blockages can be caused by inflammation, infection, surgery, or endometriosis, and sometimes clients have no symptoms until they try to conceive.
Suggestions for Fertility Coach:
Start with compassion: “Tubal concerns can feel scary, but a lot depends on whether one or both tubes are affected.” Ask what kind of testing they’ve had, such as HSG or HyCoSy. Reassure: “If even one tube is open, natural conception is still possible.” Offer a script like, “Let’s talk through what your provider saw so you understand exactly what’s happening.” Explain how sperm and egg meet inside the tubes to reduce confusion. Encourage anti-inflammatory lifestyle habits that may support pelvic health. Suggest asking their provider specific questions about which tube was blocked. Validate feelings: “It’s completely normal to feel overwhelmed—tubal issues often come as a surprise to clients.” If both tubes are blocked, compassionately guide them toward next-step options. Finish with empowerment: “No matter what the results show, you have paths forward.” -
Yes—semen analysis gives helpful information about count, motility, and morphology, but it doesn’t guarantee perfect sperm function inside the reproductive tract. Sperm must survive the vaginal environment, travel through the cervix, swim through cervical fluid, navigate the uterus, and reach the fallopian tubes. Cervical mucus quality, timing, sperm DNA integrity, and even subtle motility issues can influence this journey. A normal test reflects laboratory conditions but cannot fully replicate the complexities of natural conception. Even with normal results, sperm can still face challenges depending on the environment and timing.
Suggestions for Fertility Coach:
Start with reassurance: “A normal semen analysis is encouraging, but it doesn’t tell us everything about how sperm behave in the body.” Encourage clients to combine timing, cervical mucus awareness, and lifestyle habits to support sperm travel. Offer a script: “Sperm still need the right cervical fluid to swim efficiently—so let’s look at how your fertile window lines up.” Ask questions such as, “What did your partner’s motility percentage look like?” Recommend limiting heat exposure and supporting antioxidants even when results are normal. Normalize that this is common—many couples still struggle despite normal tests. Encourage the partner to repeat the test after 3–6 months if conception hasn’t occurred. Provide support: “You’re doing everything right; this helps us narrow down the next best steps.” End with empowerment: “A normal analysis means the foundation is strong—we’re now fine-tuning the environment.” -
Yes—ovulation simply releases the egg, but the uterus must provide a receptive environment for implantation. Issues such as a thin endometrial lining, polyps, fibroids, or inflammation can interfere with implantation even when fertilization occurs. Hormonal imbalances, poor blood flow, or unresolved infections can also affect the uterine environment. Clients often assume ovulation guarantees pregnancy, but the uterus plays a major role in supporting early embryo development. Understanding uterine anatomy helps clients appreciate all the steps needed after ovulation.
Suggestions for Fertility Coach:
Begin with validation: “You’re right—ovulation is only one step; the uterus has an equally important role.” Offer a script: “Think of the uterus as the home the embryo needs to settle into—sometimes the home needs a little support.” Ask gentle questions about menstrual symptoms, spotting, heavy cycles, or pain. Explain that lining thickness and blood flow matter for implantation. Encourage clients to discuss ultrasounds or hysteroscopy options with their provider if concerns arise. Suggest lifestyle habits that improve uterine blood flow, such as gentle movement, hydration, and reducing inflammation. Reassure that uterine issues are common and often manageable. Encourage clients to track luteal-phase symptoms for clues. End with supportive clarity: “We’re looking at everything in the reproductive system so nothing is missed.” -
Ovaries contain all the eggs a person will ever have at birth, and these eggs gradually mature and are selected for ovulation throughout reproductive life. They do not regenerate monthly—rather, they undergo a long maturation process before one is chosen for each cycle. Testes, however, produce new sperm continuously, and a full cycle of sperm development takes about 70–90 days. This means egg supply declines over time, while sperm production is ongoing but heavily influenced by health and hormonal balance. Understanding these differences helps clients see how age and lifestyle affect fertility differently for eggs and sperm.
Suggestions for Fertility Coach:
Begin with a grounding script: “Eggs are with you from birth, but sperm are made fresh all the time—they follow different biological timelines.” Use diagrams to explain follicle development and spermatogenesis. Normalize concerns about age by saying, “Egg quality can still be supported even though supply doesn’t regenerate.” Ask about lifestyle habits that affect both egg maturation and sperm production. Suggest specific supports like antioxidants, stress reduction, and consistent sleep. For sperm health, explain: “Changes you make today show up in sperm quality in about 2–3 months.” Encourage clients not to compare themselves to others—fertility timelines are highly individualized. Offer clear takeaways: “Eggs take months to mature before ovulation, and sperm are always renewing—we can support both processes.” End with empowerment: “Understanding how your body makes eggs and sperm helps you make choices that support conception.”
Female Reproductive System
Male Reproductive System
A. FOUNDATIONAL DEFINITION & EXPLANATION
Hormonal regulation is the complex system through which the brain and endocrine glands coordinate the menstrual cycle, ovulation, sperm development, and overall reproductive function. These hormones act as chemical messengers, telling the body when to prepare an egg, when to thicken the uterine lining, and when to trigger ovulation. In individuals with testes, hormones signal when to produce sperm and regulate testosterone. Even small hormonal fluctuations can influence cycle timing and fertility, which is why understanding these patterns is essential for fertility coaching. Hormones operate in a continuous feedback loop—each one influencing the next.
In ovary-bearing individuals, the menstrual cycle is divided into phases driven primarily by estrogen, progesterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH). The follicular phase begins with menstruation, during which FSH signals the ovaries to develop follicles. Rising estrogen leads to ovulation by triggering a surge of LH. After ovulation, the luteal phase begins, and progesterone prepares the uterine lining for possible pregnancy. A real-life example is imagining the cycle as a symphony: each hormone is an instrument that must play at the right time for the music (ovulation) to occur smoothly.
In individuals with testes, hormonal regulation involves the hypothalamus, pituitary gland, and testes working together to manage testosterone and sperm development. The hypothalamus releases GnRH (gonadotropin-releasing hormone), which signals the pituitary to release LH and FSH. LH stimulates testosterone production, while FSH directly supports sperm formation. If testosterone levels are too high from external supplements, the brain may reduce LH and FSH release—causing sperm counts to drop. This hormonal feedback system helps explain why lifestyle choices or supplements can affect fertility.
Hormones are sensitive to environmental factors such as sleep, stress, nutrition, exercise, and illness. For example, stress elevates cortisol, which can interfere with LH and FSH and delay ovulation. Inconsistent sleep or extreme dieting can also disrupt hormone balance. Understanding how these daily factors influence reproductive hormones helps coaches provide realistic guidance to clients. Fertility often improves simply by supporting hormone health through sustainable lifestyle habits.
Cycle coordination refers to how all hormonal changes align to create predictable patterns in the menstrual cycle or sperm development. When hormones are balanced, cycles tend to be more regular and ovulation more predictable. When hormones fluctuate irregularly—such as in PCOS, thyroid disorders, or prolonged stress—cycles may become unpredictable. Clients are often comforted when they understand the logic behind these changes. This clarity empowers them to track their cycles more effectively and seek medical evaluation when needed.
B. SCENARIOS & TIPS
Scenario 1: Client Unsure Why Ovulation Keeps Changing Each Month
Your client notices that their ovulation date varies from cycle to cycle. They worry something is “wrong” with their hormones and fear they may not ovulate regularly. They express confusion because apps often predict a fixed ovulation date. They want reassurance and a clearer understanding of cycle variability.
Coach Response
“It’s completely understandable to feel confused—many people assume ovulation happens on the exact same day each cycle because that’s how apps present it. But your body responds to real-life factors like sleep, stress, travel, and illness. These can shift the timing of ovulation even when your overall cycle is healthy. Variation doesn’t mean your hormones are ‘broken’; it just means your body is adapting.”
“I can walk you through how hormones rise and fall throughout the cycle so you can better understand what influences timing. Many clients feel more empowered once they learn how to observe physical signs such as cervical mucus changes or mid-cycle sensations. Tracking your body instead of relying solely on apps gives you a clearer picture of your own rhythm. You’re not doing anything wrong—your body is simply following its own timeline.”
Tips
This response helps clients release fear around cycle irregularity by reframing hormonal variation as normal. It emphasizes body awareness rather than rigid app predictions. Coaches should avoid diagnosing hormonal disorders unless patterns clearly warrant medical input. Encourage clients to track multiple fertility signs, including mucus, basal body temperature, or LH tests. Provide reassurance that occasional irregular cycles occur for most people. The goal is to teach clients how to observe patterns rather than expect perfect monthly consistency.
Scenario 2: Client Says Stress Has “Stopped” Their Cycle
A client reports that they have been under intense stress and have not ovulated or gotten a period for two months. They fear this is permanent or a sign of infertility. They ask if stress can truly disrupt hormones that much. They seek clarity and emotional reassurance.
Coach Response
“Your experience makes complete sense—stress can have a powerful effect on reproductive hormones. When stress levels rise, the body sometimes delays ovulation because it interprets the environment as unsafe or overwhelming. This is a temporary, protective response rather than a sign of infertility. Many people experience delayed cycles during major life transitions.”
“You’re not alone in this, and your body is not shutting down permanently. Once stress decreases, the hormonal signals that trigger ovulation often return on their own. We can focus on small, manageable strategies that support your nervous system while you navigate this period. Your cycle may take time to reestablish its rhythm, but change is absolutely possible.”
Tips
Clients often feel ashamed or frightened when stress affects their cycles. This script normalizes their experience and reduces internal blame. Coaches can help by offering grounding strategies such as consistent sleep routines, gentle movement, or setting boundaries. Avoid making promises about exactly when ovulation will return. Encourage clients to monitor their symptoms and reach out to a provider if amenorrhea continues for several months. Focus on empowerment, not pressure.
Scenario 3: Partner Unsure How Hormones Affect Sperm Quality
A partner asks why sperm counts fluctuate so much between months. They feel confused because they believed sperm production was consistent. They worry that lower results mean permanent damage. They want to understand hormonal influence on sperm health.
Coach Response
“It’s very normal to see changes in sperm count or motility from one month to the next. Sperm development takes about 72 days, and hormones like testosterone and FSH guide that process. Anything that affects hormones—sleep, heat exposure, stress, illness, exercise habits—can influence sperm quality temporarily. These shifts don’t mean something is permanently wrong.”
“Think of sperm production as a moving process rather than a fixed number. Supporting hormone balance through consistent habits can help improve outcomes, but it’s also normal to see ups and downs. Many clients find it reassuring to understand the full development cycle, and I can walk you through it step by step. You’re doing the right thing by asking and staying informed.”
Tips
This explanation reassures clients without minimizing their concerns. Coaches should emphasize that sperm quality reflects long-term patterns, not single events. Avoid interpreting medical test results; instead, focus on general education about hormone-driven fluctuation. Encourage lifestyle habits that support hormone balance, such as reducing heat exposure and maintaining consistent sleep. Reinforce that temporary dips are common and often reversible. Empower clients with knowledge rather than fear.
C. EVIDENCE-BASED INSIGHTS
Research 1: Chronic Stress and Cycle Irregularity (Armstrong et al., 2021)
Armstrong et al. (2021) investigated how chronic stress influences hormone regulation in ovary-bearing individuals. The study found that elevated cortisol interferes with the release of GnRH, which then disrupts LH and FSH—key hormones responsible for ovulation. This can lead to delayed ovulation or skipped cycles entirely. The researchers showed that even moderate stress levels over several weeks significantly shifted cycle timing. Importantly, the study also found that cycle patterns often normalized once stress was reduced. These findings validate the lived experiences of clients who notice irregular cycles during stressful periods. For fertility coaches, the research provides a biological explanation that can help clients feel reassured rather than alarmed. The study highlights stress as a modifiable factor, meaning clients can influence their reproductive health with supportive habits. It reinforces the importance of holistic care in fertility coaching.
Research 2: LH Surge Variability and Ovulation Prediction (Pillsbury et al., 2017)
Pillsbury and colleagues (2017) examined how luteinizing hormone (LH) surges vary across individuals and cycles. The study found significant differences in surge length—from a few hours to nearly two days. Some participants experienced multiple small LH rises before the true surge. This helps explain why ovulation predictor kits sometimes show confusing or inconsistent results. The researchers confirmed that ovulation typically occurs 24–36 hours after the surge peak, but emphasized that individual timing varies. These findings support teaching clients to pair LH tests with physical signs such as cervical mucus changes. The study also reassures clients that fluctuating test results do not necessarily indicate hormonal disorders. It provides a clear foundation for understanding why ovulation prediction is part science, part pattern recognition. For coaches, this research strengthens the case for flexible, body-aware fertility tracking.
Research 3: Testosterone, Supplements, and Sperm Suppression (Martinez et al., 2022)
Martinez et al. (2022) explored how external testosterone supplements influence sperm development. The study revealed that when external testosterone enters the body, the brain reduces LH and FSH production because it perceives hormone levels as already adequate. This suppresses sperm production, sometimes drastically. Participants were often surprised to learn that high testosterone levels could lower fertility rather than improve it. The research emphasized that these effects are usually reversible once supplements are discontinued. The study also highlighted the importance of avoiding non-prescribed hormone products. For fertility coaches, this evidence is essential for educating clients about hormonal balance and safe practices. It underscores how delicate the reproductive feedback system is and why external hormones must be used cautiously. The findings support open conversations about supplements, lifestyle choices, and reproductive health.
D. KEY TERMS & DEFINITIONS
Follicle-Stimulating Hormone (FSH)
FSH is a hormone produced by the pituitary gland that supports follicle development in the ovaries and sperm production in the testes. In ovary-bearing individuals, FSH helps follicles mature in preparation for ovulation. In testis-bearing individuals, it assists in the early stages of sperm formation. Abnormal FSH levels may influence cycle regularity or fertility potential. Tracking FSH trends can reveal deeper insights into reproductive function. Understanding FSH helps clients interpret hormonal patterns.
Luteinizing Hormone (LH)
LH triggers ovulation in individuals with ovaries and stimulates testosterone production in individuals with testes. The LH surge is a reliable sign that ovulation is approaching. In fertility tracking, LH tests help identify the fertile window. However, LH surges vary widely, and some cycles produce multiple small rises. Understanding LH helps clients interpret predictor kits with less confusion. Balanced LH levels support healthy reproductive function.
Estrogen
Estrogen is a hormone that regulates the first half of the menstrual cycle and helps thicken the uterine lining. It also supports cervical mucus changes that make it easier for sperm to travel. Estrogen levels rise prior to ovulation and contribute to the LH surge. Low or irregular estrogen levels can affect cycle length and fertility. Estrogen also influences mood, energy, and bone health. Its role extends beyond reproduction, affecting overall well-being.
Progesterone
Progesterone is produced after ovulation and prepares the uterine lining for implantation. It stabilizes the lining and supports early pregnancy if conception occurs. If pregnancy does not occur, progesterone levels drop and menstruation begins. Low progesterone may contribute to short luteal phases or implantation difficulties. Clients often track progesterone trends to understand their cycle better. Progesterone is also known for its calming, stabilizing effects on the body.
Testosterone
Testosterone supports libido, energy, and reproductive function in testis-bearing individuals. It works alongside FSH to stimulate sperm development. Testosterone levels fluctuate daily and can be influenced by stress, sleep, and lifestyle factors. Excess external testosterone suppresses sperm production due to hormonal feedback loops. Balanced testosterone supports fertility and overall health. Understanding testosterone helps explain why lifestyle shifts can improve sperm quality.
2. Hormonal Regulation & Cycle Coordination
FAQs: Hormonal Regulation & Cycle Coordination
-
Hormones like FSH, LH, estrogen, and progesterone work together in a carefully coordinated cycle to trigger ovulation and prepare the uterus for pregnancy. Early in the cycle, FSH stimulates follicle growth, leading estrogen to rise; this rise signals the body to release LH, which triggers ovulation. After ovulation, progesterone increases to stabilize the uterine lining and support potential implantation. If no pregnancy occurs, hormone levels fall, causing menstruation to begin and the cycle to restart. Understanding this system helps clients grasp why timing is crucial and why slight hormonal misalignments can delay or prevent ovulation.
Suggestions for Fertility Coach:
Use simple language when explaining hormone interactions, such as, “Think of your hormones as a relay team—each one hands off to the next to make ovulation happen.” Offer visual aids or charts to show the predictable rise and fall of hormones. Encourage clients to track their cycle using ovulation predictor kits, basal body temperature, or cervical mucus changes. Provide a script like, “Your estrogen rising tells us ovulation is coming—your LH surge confirms it’s almost here.” Normalize variations: “It’s okay if your hormones shift a little each month; your body isn’t a machine.” Suggest lifestyle supports like sleep, stress reduction, and nutrient intake to balance hormones naturally. Ask gentle clarifying questions: “Have you noticed patterns in your cycles, like early ovulation or longer luteal phases?” Offer reassurance when cycles seem irregular. Empower clients by reminding them, “Once we understand your hormone patterns, we can time your fertile window with much more confidence.” -
Irregular cycles can occur for many reasons, including stress, hormonal imbalances, thyroid issues, PCOS, rapid weight changes, or disrupted sleep patterns. Irregularity does not automatically mean someone isn’t ovulating—it may mean ovulation is inconsistent or delayed. When ovulation timing varies, cycles become harder to track and fertile windows shift month to month. Some cycles may have a long follicular phase, meaning it takes longer for estrogen and FSH to align for ovulation. Understanding these causes helps clients avoid assuming infertility and instead approach testing and tracking with clarity.
Suggestions for Fertility Coach:
Start by validating the client: “Irregular cycles are extremely common, and they don’t automatically mean anything is wrong.” Help them understand that tracking ovulation—not period dates—is the best indicator of fertility. Suggest practical tracking tools like LH tests or BBT charts. Offer a script such as, “Let’s focus on identifying whether ovulation is happening rather than the exact length of your cycle.” Encourage screening for thyroid, insulin resistance, and hormone levels if patterns suggest deeper imbalance. Reassure clients by saying, “Many people with irregular cycles become pregnant once we understand their ovulation pattern.” Teach them how stress and routines influence the hypothalamus–pituitary–ovarian axis. Introduce small habit changes: consistent sleep, balanced blood sugar, and meal timing. Ensure they feel supported by ending with, “You’re not alone in this—irregular cycles are something we can absolutely work through together.” -
The fertile window refers to the six-day period ending on the day of ovulation, when estrogen levels rise and create an environment conducive to sperm survival. As estrogen climbs, it produces fertile-quality cervical mucus that helps sperm move efficiently. The LH surge occurs about 24–36 hours before ovulation and is the strongest hormonal indicator that the fertile window is about to close. Progesterone rises after ovulation and signals the shift into the non-fertile, luteal phase. Clients often misunderstand this timing, so understanding hormone patterns helps clarify when intercourse is most effective.
Suggestions for Fertility Coach:
Use everyday language such as, “Your fertile window is when your hormones create the perfect setting for sperm and egg to meet.” Show clients visuals of how estrogen rises before ovulation and how LH predicts the exact timing. Provide a script like, “When your LH test turns positive, that means ovulation is coming soon, so today and tomorrow are your best days to try.” Encourage clients to observe fertile cervical mucus as another signal. Recommend keeping a simple cycle log or using a tracking app. Gently correct misconceptions like, “You aren’t fertile for the whole month—just a specific few days.” Offer reassurance when timing feels stressful: “It takes practice to learn your body’s signs. You’re doing great.” Guide couples through communication about timing so it feels less pressured. Remind clients that missing one fertile window isn’t harmful: “Every cycle is a new opportunity, and your body gives us signals each time.” -
Hormones naturally fluctuate across the menstrual cycle, so changes in mood, energy, and physical sensations are expected. Estrogen typically boosts energy and libido during the follicular phase, while higher progesterone after ovulation can lead to increased tiredness, bloating, or emotional sensitivity. When hormones rise or fall too quickly, clients may experience PMS, anxiety, breast tenderness, or sleep disruptions. Chronic stress, under-eating, and blood sugar instability may intensify these symptoms by affecting the hormone-regulating centers in the brain. Understanding the hormonal rhythm helps clients track how symptoms correlate with each phase of their cycle.
Suggestions for Fertility Coach:
Normalize symptoms by saying, “Your hormones influence more than fertility—they can impact mood, energy, and the way your body feels.” Encourage clients to track symptoms alongside ovulation patterns to identify trends. Provide practical habits such as balanced meals, magnesium, hydration, and better sleep routines. Offer a script like, “If you notice fatigue or irritability after ovulation, that’s a progesterone-related shift, not something you’re doing wrong.” Suggest stress-reduction practices like breathwork, soft movement, or mindful breaks. Educate clients on when symptoms may indicate deeper issues that require medical evaluation (thyroid, PCOS, PMDD). Remind them: “Your body is responding to hormone changes—it’s not a character flaw or weakness.” Coach them on self-compassion during tougher phases. Encourage journaling or cycle-syncing strategies to help manage expectations and energy levels. End with reassurance: “By understanding these patterns, we can help you feel more supported and more in control.” -
Male fertility is regulated by a hormonal system similar to the female cycle, led by the hypothalamus and pituitary gland. FSH stimulates sperm production in the testes, while LH signals the testes to produce testosterone, which supports healthy sperm development. Disruptions in these hormones can reduce sperm count, motility, or morphology. Stress, poor sleep, obesity, excessive heat, and certain medical conditions can influence hormonal balance. Understanding male hormonal patterns helps clients see fertility as a shared process influenced by both partners’ health.
Suggestions for Fertility Coach:
Use inclusive language such as, “Just like eggs need the right hormones, sperm do too—and the good news is that sperm can improve quickly.” Encourage male clients to consider a semen analysis early on. Provide practical steps like better sleep, reduced alcohol, improved diet, and limiting heat exposure. Use a script such as, “FSH helps the body make sperm, and LH helps produce the testosterone that supports healthy sperm development.” Normalize concerns: “You’re not alone—hormones affect male fertility more than most people realize.” Suggest stress reduction since cortisol directly impacts testosterone. Recommend simple tracking methods: energy levels, libido, or changes in stress. Encourage open communication between partners: “It can really help to approach this as a team.” Remind clients that sperm regeneration takes about 70–90 days, so improvements take time but are absolutely possible. Offer steady reassurance that positive changes often yield noticeable gains.
What is FSH and what is its role in my fertility?
Hormones: Are Your Hormones Normal?
3. How Reproduction Supports Conception
A. FOUNDATIONAL DEFINITION & EXPLANATION
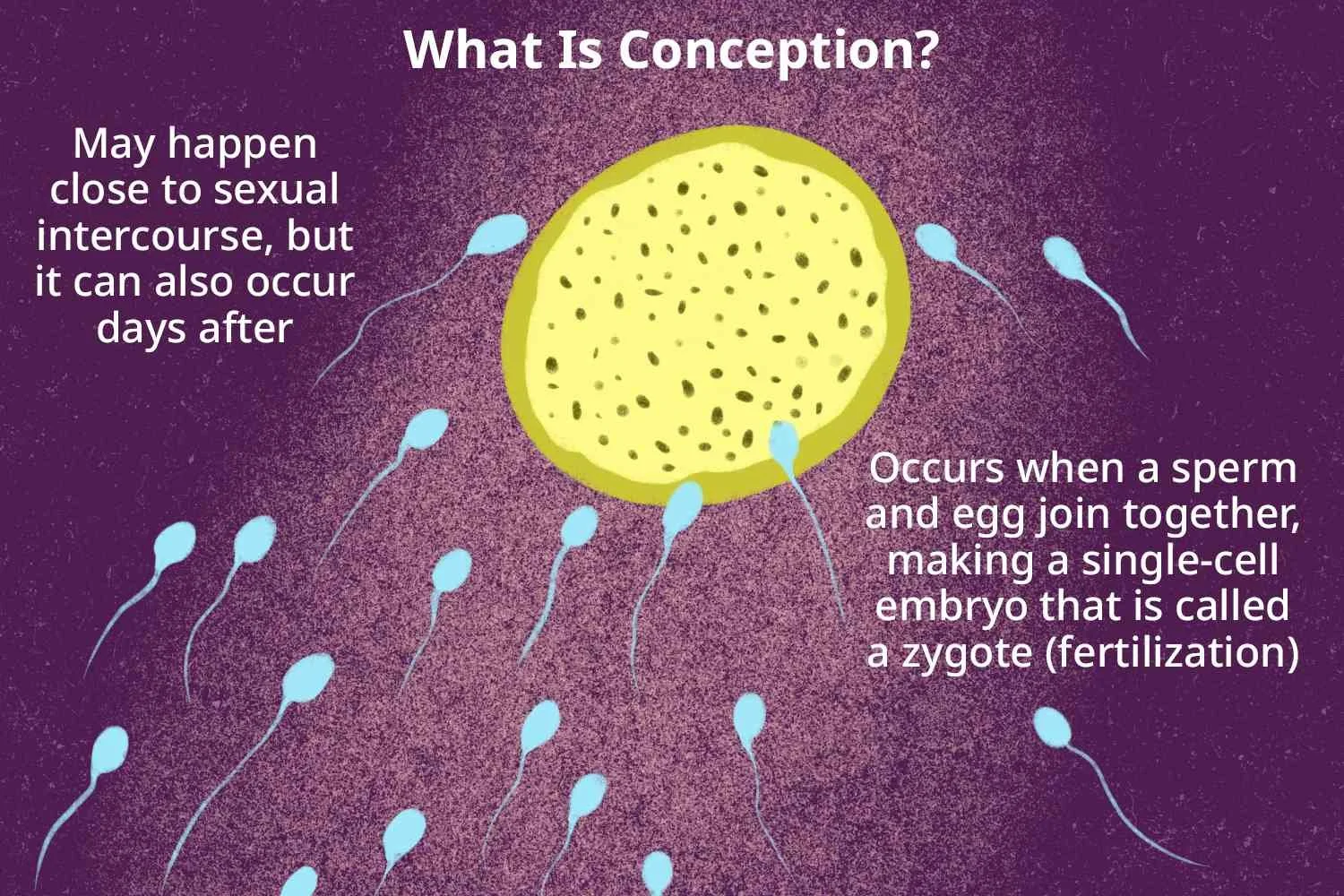
Conception is the result of a series of coordinated biological events that involve both reproductive anatomy and hormonal timing. For conception to occur, sperm must reach and fertilize a mature egg, and the resulting embryo must implant successfully in the uterus. Each step in this process depends on optimal conditions in both partners, though “optimal” varies widely among individuals. Understanding these steps helps clients recognize what is typical, what varies, and what may require medical insight. For fertility coaches, explaining conception in simple, practical terms empowers clients and helps reduce fear or self-blame.
Conception begins with ovulation—the release of a mature egg from the ovary. The egg then travels into the fallopian tube, where it remains viable for about 12–24 hours. Sperm, however, can survive in fertile cervical mucus for up to five days. This difference explains why intercourse does not need to happen exactly on the day of ovulation for pregnancy to occur. A helpful way to visualize this is to imagine the egg as a limited-time “event,” while sperm act more like early-arriving guests waiting for the main moment.
Once sperm enter the reproductive tract, they must navigate cervical mucus, the uterus, and the fallopian tubes. Only a fraction of sperm reach the tube, and only one will ultimately penetrate the egg. Cervical mucus plays a key role in filtering out lower-quality sperm while supporting the strongest swimmers. Meanwhile, the fallopian tube provides an environment that aids fertilization and early embryo development. This selective, supportive process highlights how reproduction naturally favors healthy sperm and promotes genetic stability.
After fertilization, the embryo begins dividing and traveling toward the uterus, where it seeks a place to implant. The uterine lining, thickened by progesterone during the luteal phase, provides nourishment and structure for implantation. Not every fertilized egg implants successfully—this is a normal part of reproduction, not a sign of failure. Many early pregnancies end before a person even realizes conception occurred. This reality helps clients understand why even well-timed cycles do not always lead to pregnancy.
Successful conception is influenced by many factors beyond timing, including cycle regularity, anatomy, sperm health, cervical mucus quality, and uterine environment. Lifestyle factors such as stress, sleep, and nutrition can also support or disrupt reproductive function. Coaches play a key role in helping clients understand these elements without overwhelming them. The goal is not to create pressure to perfect every factor but to guide clients toward simple, sustainable habits that support reproductive health. When clients understand the biological logic behind conception, they often feel more confident and less anxious throughout the process.
B. SCENARIOS & TIPS
Scenario 1: Client Confused Why Pregnancy Hasn’t Happened Despite “Perfect Timing”
Your client says they timed intercourse precisely around ovulation, used ovulation predictor kits, and monitored cervical mucus. They feel discouraged because pregnancy did not occur despite doing “everything right.” They worry they are failing or missing something important. They turn to you for clarification and reassurance.
Coach Response
“It’s completely understandable to feel discouraged when you’ve done everything you can to optimize timing. Even with perfect timing, the chance of conception each cycle for most couples is around 20–25%. That means several cycles are often needed, even when everything is functioning normally. Your body is not failing—this is simply how human reproduction works.”
“We can talk through all of the steps involved in conception to help you better understand why timing alone doesn’t guarantee pregnancy. Things like embryo quality, implantation, and hormonal alignment all play a role behind the scenes. You’re taking thoughtful steps, and that matters. We can continue to support your awareness without placing pressure or blame on yourself.”
Tips
This response relieves pressure by reframing conception probabilities in realistic terms. Coaches should emphasize that multiple cycles are normal and expected. Avoid suggesting that “trying harder” will increase success. Instead, encourage sustainable tracking habits and emotional support. Reinforce that the client’s efforts are valid but that biology is complex. This helps reduce anxiety and promotes a healthier mindset.
Scenario 2: Client Asking Why Cervical Mucus Matters for Conception
A client has heard about tracking cervical mucus but finds it “gross,” confusing, or difficult to interpret. They do not understand why mucus changes affect conception. They also feel unsure whether they are identifying fertile mucus correctly. They want a simple explanation.
Coach Response
“Cervical mucus may feel strange to talk about, but it plays a major role in supporting sperm on their way to the egg. During your fertile window, mucus becomes clearer, stretchier, and more slippery—almost like raw egg whites. This texture allows sperm to swim more efficiently and survive longer. Outside the fertile window, mucus becomes thick and creates a barrier.”
“Learning to observe these changes can help you understand when your body is getting closer to ovulation. It doesn’t have to be complicated or perfect—just understanding general patterns can be incredibly helpful. Think of cervical mucus as your body’s natural signal that conditions are ideal for conception. If you want, I can help you explore simple ways to identify those changes.”
Tips
This explanation uses accessible language, reducing embarrassment or confusion. Coaches should normalize all client reactions to discussing mucus. Avoid overly clinical descriptions; use practical analogies instead. Encourage clients to focus on patterns rather than perfection. Reassure them that variability is normal and that learning takes time. Always keep the tone supportive, not pressured.
Scenario 3: Partner Confused Why Sperm Quality Matters If “Only One Sperm” Fertilizes the Egg
A partner believes sperm quality doesn’t matter because they think only one sperm is needed. They don’t understand the role of overall sperm health, count, and motility. They worry they might be the reason conception hasn’t occurred but feel unsure how to support improvement. They seek guidance without shame.
Coach Response
“It’s true that one sperm fertilizes the egg, but many sperm work together to make that happen. The first group helps break down cervical mucus, another group helps guide the path to the egg, and the strongest swimmers reach the fallopian tube. Having more healthy sperm increases the likelihood that one will reach the egg at the right moment. It’s a coordinated effort, not a single-event race.”
“Small lifestyle habits—like reducing heat exposure, getting consistent sleep, staying hydrated, or managing stress—can support healthier sperm. The good news is that sperm regenerate every 72 days, so positive changes can lead to improvements over time. You’re not alone in this, and asking these questions is an important first step. I can help you explore simple adjustments without pressure.”
Tips
This explanation supports understanding while removing guilt. It uses clear examples that illustrate why sperm quality matters. Coaches should avoid implying that low-quality sperm are the sole cause of fertility challenges. Encourage small, realistic habits rather than drastic changes. Reinforce the regenerative nature of sperm to inspire hope. Support openness and shared responsibility between partners.
C. EVIDENCE-BASED INSIGHTS
Research 1: Cervical Mucus and Sperm Protection (Haddad et al., 2020)
Haddad et al. (2020) investigated how cervical mucus supports sperm survival during the fertile window. The study found that fertile cervical mucus becomes less acidic and more alkaline, creating a protective environment for sperm. This mucus also helps filter out lower-quality sperm, allowing only the strongest swimmers to progress. The researchers noted that mucus consistency dramatically influences sperm mobility. Thicker or less fertile mucus was associated with significantly lower sperm survival rates. The study helps explain why some cycles with the same timing may lead to different results. For clients, it provides clarity about why mucus observation is important. This research supports teaching clients to recognize fertile patterns. It reinforces cervical mucus as a major factor in successful conception.
Research 2: Sperm Transport Timing (Lee et al., 2016)
Lee and colleagues (2016) examined the speed at which sperm travel through the reproductive tract. The study found that sperm can reach the fallopian tubes within minutes, though many take several hours. This helps explain why intercourse several days before ovulation can still result in pregnancy. The research also showed that cervical mucus acts as both a guide and a filter. Only the most motile sperm pass effectively through the cervix. The study highlighted the importance of sperm resilience and overall semen quality. It reassures clients that conception does not always require exact, same-day timing. For coaches, this provides evidence to support more flexible fertility guidance. The findings help clients understand why conception is possible across a range of timing scenarios.
Research 3: Egg Quality, Age, and Conception Outcomes (Rubens et al., 2018)
Rubens et al. (2018) explored how egg quality changes with age and how those changes impact conception. The study found that while egg quantity decreases predictably over time, egg quality follows a more gradual and variable pattern. Many individuals over 35 successfully conceive without intervention. The researchers emphasized that lifestyle factors such as diet, stress, and exercise influence egg health. They also highlighted the role of mitochondrial function in egg development. Age-related changes do not mean infertility; they reflect natural shifts in reproductive biology. For clients, this research offers reassurance and perspective. Coaches can use these findings to promote a balanced, non-alarmist discussion about age and fertility. It supports a compassionate, evidence-based approach to fertility education.
D. KEY TERMS & DEFINITIONS
Fertilization
Fertilization occurs when a sperm penetrates the egg, forming a zygote. This typically happens within the fallopian tube. Only one sperm fertilizes the egg, but many contribute to the process by clearing the path. Fertilization triggers cell division and early embryo development. This step marks the very beginning of pregnancy. Understanding fertilization helps clients visualize the process behind conception.
Implantation
Implantation happens when the developing embryo attaches to the uterine lining. This usually occurs 6–10 days after ovulation. Progesterone supports the uterine lining to make implantation possible. Not every fertilized egg implants successfully, which is a normal part of reproduction. Implantation determines whether pregnancy continues. Understanding this helps clients interpret early pregnancy symptoms.
Embryo
An embryo is the early stage of human development from fertilization through the first eight weeks. During this time, the cells divide rapidly and begin forming essential structures. The embryo travels from the fallopian tube to the uterus. Implantation occurs during the embryonic stage. Embryo quality influences whether pregnancy will continue. Understanding the embryo helps clients contextualize early pregnancy outcomes.
Cervical Mucus
Cervical mucus is a fluid produced by the cervix that changes throughout the menstrual cycle. Fertile mucus becomes clear, stretchy, and slippery, helping sperm travel and survive. Non-fertile mucus becomes thicker and blocks sperm passage. Mucus patterns provide valuable insights into timing and fertility. Tracking mucus is one of the most reliable natural indicators of ovulation. It’s an essential part of conception awareness.
Sperm Motility
Sperm motility refers to how well sperm move. Strong, forward movement helps sperm travel through cervical mucus and reach the egg. Poor motility can reduce the chances of successful fertilization. Motility fluctuates based on health, lifestyle, and hormonal changes. Supporting motility often involves simple lifestyle adjustments. Understanding motility helps clients interpret general fertility concepts.
FAQs about how Reproduction Supports Conception
-
Ovulation is necessary for pregnancy, but it must align with sperm availability, sperm quality, and cervical fluid conditions for fertilization to occur. Even in perfectly healthy couples, the chance of conception each cycle is only about 20–25%, meaning most cycles naturally don’t result in pregnancy. Sometimes the egg may not be of optimal quality, or sperm may not reach the egg during the short 12–24 hour window the egg is viable. Cervical fluid may also not be fertile enough that month to support sperm travel. Cycle timing variations and normal hormonal fluctuations can also lead to missed opportunities even when ovulation technically occurs.
Suggestions for Fertility Coach:
Normalize this experience using a script like, “Ovulation gives us the opportunity, but many factors must align at the same moment—it doesn’t mean anything is wrong.” Encourage the client to track ovulation more precisely using LH tests, cervical fluid, and symptoms. Suggest timing intercourse 1–2 days before ovulation, not just on ovulation day. Reassure: “Most conception happens from sperm waiting for the egg—not the other way around.” Ask gentle assessment questions like, “What did you notice in your cervical mucus this cycle?” Educate about sperm survival in fertile mucus to reduce pressure. Encourage consistent healthy habits that impact egg quality, stress, and cycle regularity. Validate emotions: “It’s completely normal to feel confused or frustrated—many clients experience this before they conceive.” End with empowerment: “You did things right this cycle; you’re gathering information that will help us refine timing even more.” -
LH (luteinizing hormone) can fluctuate throughout the day and may show multiple rises before the true surge that triggers ovulation. This can happen due to stress, irregular cycles, weaker hormone signaling, or natural hormonal variations. Some people have short surges that are easy to miss, and others experience “false starts” before the final peak. Even with fluctuating LH, ovulation can still occur normally. Understanding the body’s patterns—alongside cervical mucus and temperature shifts—gives a fuller picture of whether ovulation is happening.
Suggestions for Fertility Coach:
Start by validating their confusion: “LH tests can be tricky—your body isn’t malfunctioning; it’s just communicating in its own rhythm.” Teach clients to test LH twice daily during suspected fertile days. Offer the script: “Look for the darkest test in the series—that’s usually your true surge.” Encourage pairing LH tests with cervical fluid observations for more accuracy. Explain, “Your fertile mucus increasing often tells us ovulation is close, even before the LH test peaks.” Reassure them that hormone fluctuations are normal and don’t automatically indicate infertility. Suggest stress management strategies, as stress can cause multiple surges. Ask reflective questions like, “Has anything changed this month with sleep, travel, or routine?” For persistent confusion, teach them how to track retroactively using basal body temperature. End with encouragement: “You’re reading your body correctly—we just need to combine a few signs to see the full pattern.” -
Not everyone experiences textbook “egg-white” cervical mucus, even in healthy, fertile cycles. Cervical fluid varies widely in texture, color, and quantity based on hormones, hydration, stress, medications, and underlying health. Some people produce more creamy or watery fertile fluid rather than stretchy strands. As long as mucus becomes more slippery, lubricative, or wetter before ovulation, it can still support sperm survival and transport. The absence of perfect “egg-white” mucus doesn’t automatically mean poor fertility or a cycle problem.
Suggestions for Fertility Coach:
Normalize variations with the script: “Egg-white mucus is just one version of fertile fluid—your body’s version may look different and still be healthy.” Teach clients to focus on sensation (“slippery,” “wet”) rather than appearance alone. Encourage hydration and healthy fats to support mucus quality. Suggest observing mucus throughout the day—not only during bathroom visits. Validate concerns: “You’re not doing anything wrong; your mucus pattern is unique to you.” Offer guidance on avoiding vaginal irritants that can reduce mucus quality. Provide education: “Watery mucus is just as fertile—it often appears right before ovulation.” Recommend tracking mucus over several cycles for patterns. Ask clarifying questions like, “What changes do you notice right before your LH peak?” Reinforce confidence: “Your body is giving us cues—we just need to learn your personal version.” -
ven with ideal timing, several biological processes must align for sperm to reach and fertilize the egg. Sperm need to be strong enough to swim through cervical fluid, survive the journey, and undergo changes that enable fertilization. Cervical fluid must be supportive, and the egg must be healthy enough to attract and bind to a sperm cell. Cycle variability, sperm quality, egg maturity, or mucus conditions can influence each step. Conception often takes multiple cycles because the body recalibrates slightly each month.
Suggestions for Fertility Coach:
Start by reassuring: “Perfect timing doesn’t guarantee fertilization—there are many small steps happening behind the scenes.” Encourage a semen analysis if not already done. Offer practical suggestions like improving sperm motility through lifestyle tweaks. Ask, “How often did you see fertile mucus before ovulation?” Teach clients that intercourse every 1–2 days during the fertile window increases chances. Reduce pressure by saying, “It’s not about doing more—it’s about letting your body sync this process naturally.” Discuss hydration, blood sugar balance, and stress management to support mucus and hormone quality. Remind clients that fertilization rates are naturally low per cycle. Provide supportive language: “You’re doing everything right—sometimes the body just needs time.” Offer an individualized plan based on their patterns. -
Ovulation can feel different from month to month, depending on hormonal shifts, stress levels, sleep quality, and overall health. Some cycles produce a dominant follicle that creates noticeable ovulation pain or changes, while other cycles are quieter but still healthy. Egg quality, follicle size, and estrogen levels can all influence physical sensations. A “quiet” ovulation doesn’t mean ovulation didn’t happen—it may simply be less perceptible that month. These variations are part of normal reproductive functioning.
Suggestions for Fertility Coach:
Normalize it with a script like, “Ovulation isn’t supposed to feel the same each month—your body responds differently based on many small factors.” Encourage tracking multiple signs so clients don’t rely only on sensations. Teach them to observe LH peaks and cervical mucus patterns for clarity. Ask reflective questions such as, “What was happening in your life during the cycles that felt different?” Discuss how stress, illness, or travel can change ovulation symptoms. Reassure: “Quiet ovulation can still be healthy and fertile.” Suggest gentle cycle-supportive habits—consistent meals, hydration, and sleep. Provide a grounding script: “The goal isn’t to feel ovulation—it’s to understand your pattern.” Offer guidance on what would warrant a provider evaluation (e.g., no ovulation for several months). End with encouragement: “Your body still ovulates even when you don’t feel it—your signals simply vary, and that’s normal.”
Conception Explained
Fertilization
👉 Knowledge Check
-
The reproductive organs work together through a coordinated hormonal and structural system that supports conception.
Understanding both male and female anatomy helps clarify where fertility challenges may arise.
A basic knowledge of anatomy builds a foundation for interpreting symptoms, cycles, and reproductive health.
-
“Female Genital System”
Summary: This article gives a comprehensive overview of female reproductive anatomy, embryology, and physiology, explaining how structures like the ovaries, fallopian tubes, uterus and external genitalia develop and function. It highlights tissue-level changes across the menstrual cycle and the interplay between anatomy and hormonal regulation.
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7158333/“Physiology of the Female Reproductive System” — StatPearls (NBK book chapter)
Summary: This source breaks down the anatomical components (internal and external) of the female reproductive system, describes the histology of each region, and connects structural features to their hormonal functions (e.g., estrogen, progesterone). It’s a reliable educational overview used for clinical anatomy and physiology.
Link: https://www.ncbi.nlm.nih.gov/books/NBK537132/“Endocrinology of the Male Reproductive System and Spermatogenesis” chapter.
Summary: This chapter explores the male reproductive anatomy (testes, epididymis, ductal system, accessory glands), the hormonal regulation via the HPG axis, and how structure supports the function of sperm production and delivery. It’s readily accessible and solid for anatomical-physiological context.
Link: https://www.ncbi.nlm.nih.gov/books/NBK279031/“Female Reproductive Organ Anatomy” — Medscape Reference article
Summary: A detailed anatomy reference that describes internal and external female reproductive organs (ovaries, fallopian tubes, uterus, cervix, vagina, vulva), outlines their anatomical relationships and clinical relevance. While not a peer-reviewed journal article, it is medically accurate and useful for anatomy foundation.
Link: https://emedicine.medscape.com/article/1898919-overview
-
The timing of the “fertile window” in the menstrual cycle: day specific estimates from a prospective study.
Wilcox, A. J., Dunson, D. B., & Baird, D. D. BMJ, 2000.
This classic prospective cohort study uses daily hormone measurements to pinpoint when the six-day fertile window actually occurs in real women’s cycles. It shows that the fertile window is highly variable, even among women with “regular” cycles, and challenges the simple idea that ovulation always happens on day 14.
Link: https://pmc.ncbi.nlm.nih.gov/articles/PMC27529/
Real-world menstrual cycle characteristics of more than 600,000 menstrual cycles.
Bull, J. R., Rowland, S. P., Scherwitzl, E. B., et al. npj Digital Medicine, 2019.
Using app-tracked data from hundreds of thousands of cycles, this paper describes typical and atypical cycle lengths, follicular and luteal phase durations, and how these patterns change with age and BMI. The authors demonstrate that ovulation timing and phase length vary much more than many standard “textbook” descriptions suggest, which is crucial context for teaching fertile windows and cycle variations.
Link: https://www.nature.com/articles/s41746-019-0152-7
Cervical mucus patterns and the fertile window in women without known subfertility: a pooled analysis of three cohorts.
Najmabadi, S., Schliep, K. C., Simonsen, S. E., et al. Human Reproduction, 2021.
This pooled analysis of over 2,400 ovulatory cycles looks at how cervical mucus changes across the cycle and how many days per cycle are truly “potentially fertile.” It confirms that estrogen-driven, stretchy, slippery mucus aligns closely with higher day-specific probabilities of conception and provides concrete numbers for the length and variability of fertile days.
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8487651/
Menstrual cycle length and modern living: a review.
Campbell, L. R., & McGrath, R. T. Reproduction and Fertility, 2021.
This review summarizes how biological, lifestyle, and environmental factors (stress, nutrition, shift work, endocrine disruptors, etc.) influence menstrual cycle length and regularity. It’s useful background for explaining why some clients have very predictable cycles while others experience frequent variation—and how these differences affect identifying the fertile window.
Link: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8631146/